Embarking on the journey of physical rehabilitation begins with the Physical Therapy Assessment Form, a crucial step in devising a personalized treatment plan. This comprehensive guide, enriched with examples, delves into the creation, utilization, and interpretation of the form. It’s tailored to meet the needs of healthcare professionals and patients alike, ensuring an accurate and effective assessment process. By integrating the Physical Assessment Form and Assessment Form terminologies, we aim to provide an enriching resource that enhances understanding and application in clinical settings.
Physical Therapy Assessment Form Bundle
What is a Physical Therapy Assessment Form?
The Physical Therapy Assessment Form is a foundational tool used by therapists to evaluate a patient’s current physical condition, identify areas of concern, and establish a tailored treatment plan. It encompasses a detailed examination of the patient’s mobility, strength, balance, and functional capabilities. This form serves as a critical first step in physical therapy, enabling therapists to document baseline data, set goals, and track progress over time.
Physiotherapy Assessment Format
-
Patient Identification
- Name, Date of Birth, Gender, Contact Information, and Emergency Contact.
-
Medical and Therapy History
- Include details about previous injuries, surgeries, current medications, and any known allergies.
-
Assessment Reason
- Document the main reason for the patient’s visit and any specific complaints.
-
Physical Examination
- Record observations regarding pain intensity, affected areas, mobility, muscle strength, and any functional limitations.
-
Treatment Goals and Plan
- Define short-term and long-term rehabilitation goals based on the assessment findings. Outline the proposed treatment interventions, including types of therapy and expected frequency of sessions.
-
Professional Notes
- Provide space for the therapist’s observations, potential adjustments to the treatment plan, and any recommended exercises for the patient to perform at home.
Physical Therapy Assessment Form PDF
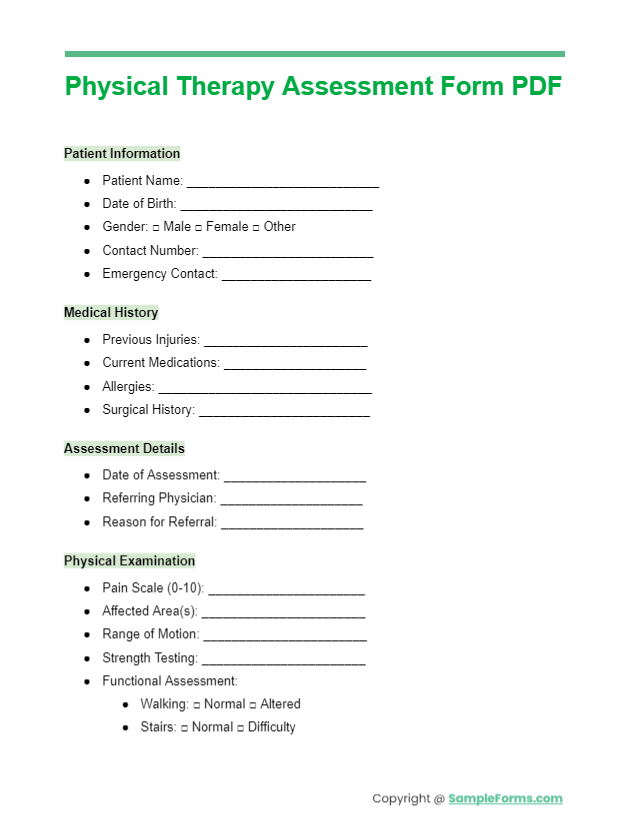
The Physiotherapy Assessment Form PDF is a digital tool designed for efficient patient evaluation, integrating seamlessly with the Self-Assessment Form, allowing patients to contribute to their own evaluation process. You should also take a look at our Nursing Assessment Form.
Physical Therapy Assessment Sheet
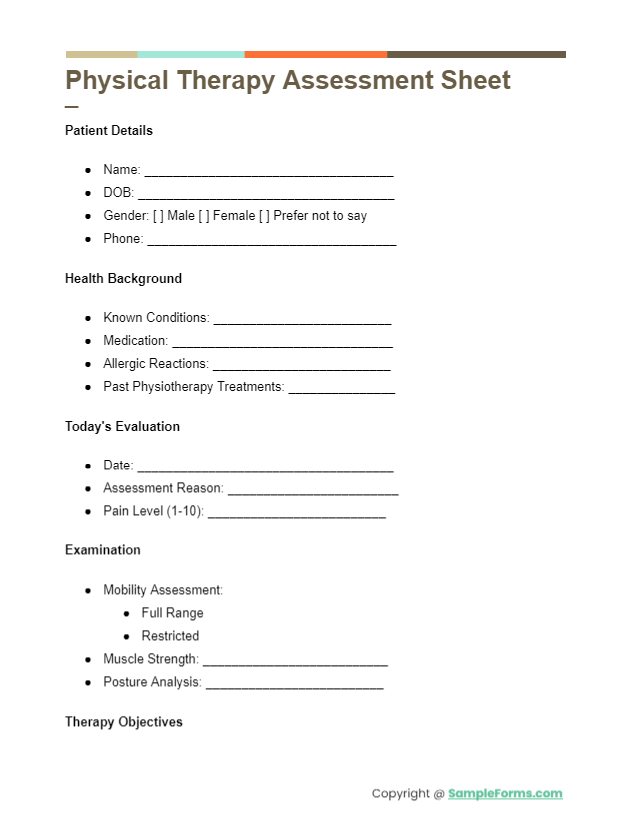
A comprehensive Physical Therapy Assessment Sheet facilitates detailed patient analysis, incorporating the Employee Assessment Form to ensure therapists’ professional skills are continuously updated and applied effectively. You should also take a look at our Interview Assessment Form.
Physical Therapy Evaluation Template
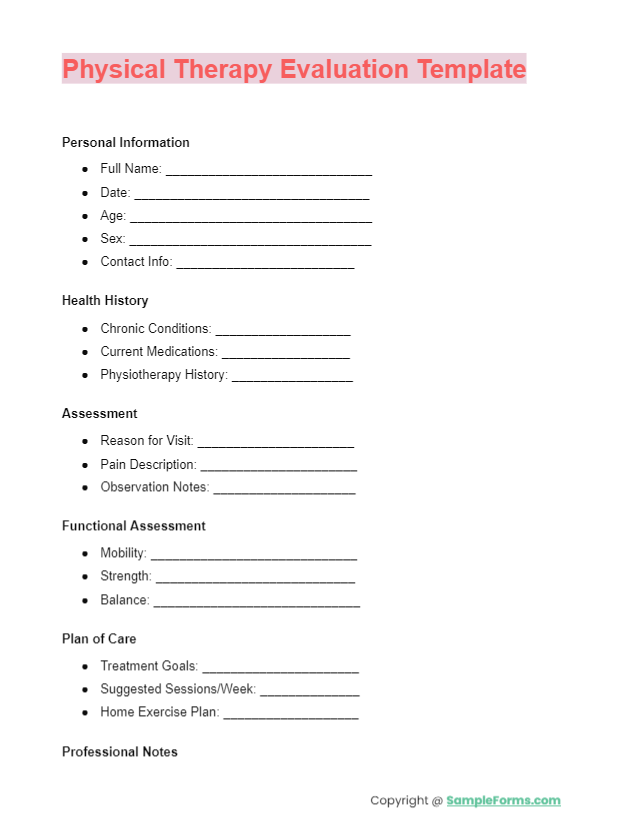
This Physical Therapy Evaluation Template serves as a structured guide for therapists, featuring elements of the Client Assessment Form to personalize treatment plans and enhance patient care from the initial visit. You should also take a look at our Risk Assessment Form.
Printable Physiotherapy Assessment Form
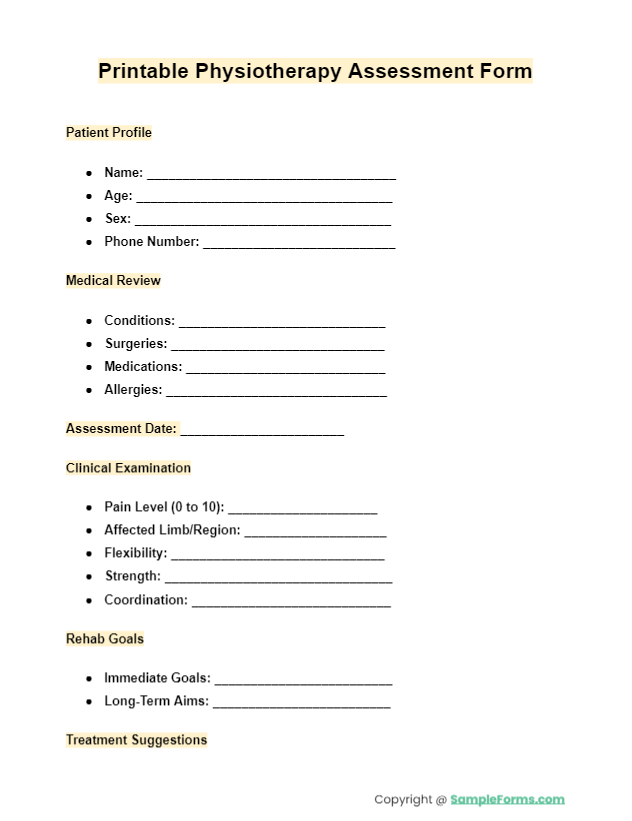
More Physical Therapy Assessment Form Sample
Physical Therapy Assessment Form Sample
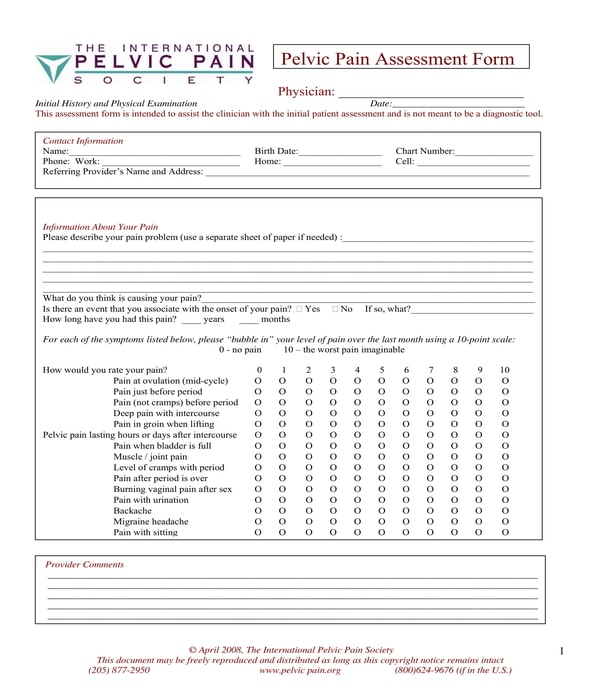
Physical Therapy Pelvic Pain Assessment Form
Examples of Physical Therapy Assessment Forms
There are several varieties of physical therapy assessment forms based on what therapists will be needing to obtain and document from their patients. Below are some examples of the forms that therapists and their patients can use:
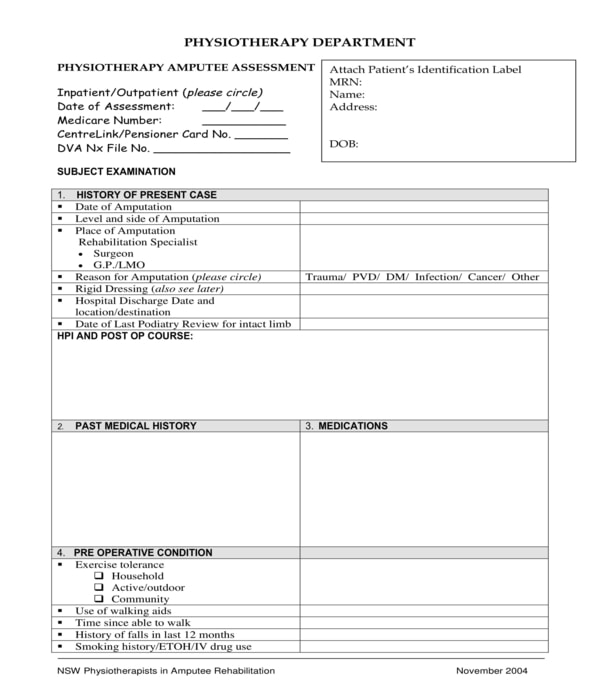
Physical Therapy Amputee Assessment Form – For patients who had limbs amputated, a physical therapist will be using a physical therapy amputee assessment form. In this form, the name of the patient, the date of his assessment, the patient’s Medicare and pensioner card number, as well as the patient’s residential address and date of birth will be stated in the first section. The succeeding section is for the patient’s history of his present case or his amputee wherein the date when the patient acquired the amputation will be disclosed along with the level and side of the amputation, the place of amputation, and the reason for the amputation.
Physical Therapy Amputee Assessment Form
The other sections of a physical therapy amputee assessment form will be for acknowledging the patient’s medical history, the medications, and treatments that the patient took and is taking, the pre-operative condition of the patient, and the patient’s social behavior and history. In addition, there are also sections for documenting the level of pain that the patient is feeling due to his amputation, the sensations that the patient has to his amputation, and the goals which are planned for the patient by his physician, surgeons, and other health care providers.
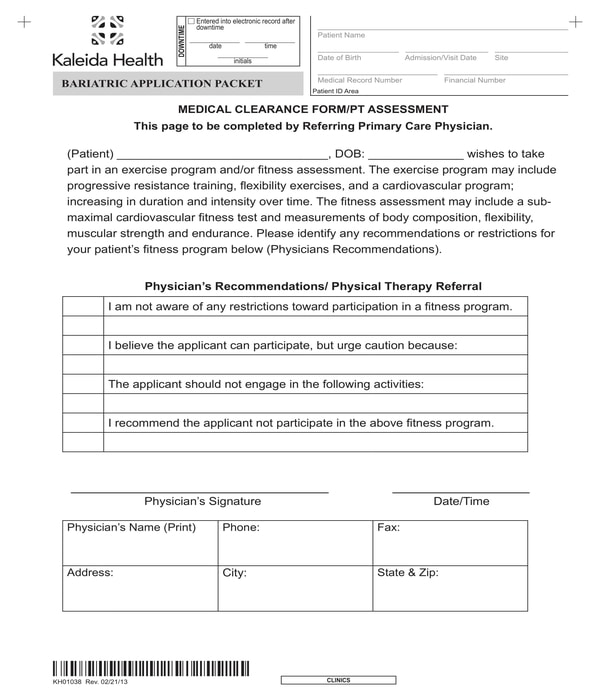
Physical Therapy Assessment Medical Clearance Form – For patients who plan to participate in an activity, specifically a rigorous activity, they must have the approval of their physical therapist documented in a physical therapy assessment medical clearance form. The purpose of the form is to prove that the patient has received the go signal or the approval of his physician in lieu of his intent in being part of the activity even with his physical issues and conditions.
Physical Therapy Assessment Medical Clearance Form
A physical therapy assessment medical clearance form will not only have the general information of the patient but also a statement which indicates the participation of the patient to a specified activity. Then, a physician recommendation or a physician referral section will have to be filled out by the patient’s therapist or physician. This is the section where the observations and the recommendations of the administering physician will be indicated along with the explanations of the patient’s limitations in relation to his condition. Lastly, to complete the form, the physician or the therapist must affix his signature on the form and disclose his name, phone number, office address, and the fax number of his office for purposes which are directly connected to sending and receiving notice forms about the patient.
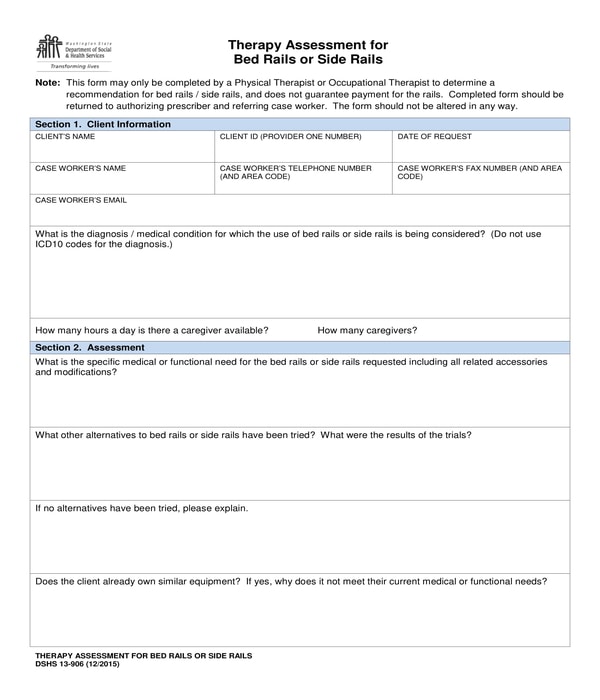
Physical Therapy Bed Rails Assessment Form – Bed rails and side rails are beneficial for patients who are in need of materials and instruments to aid them in standing and sitting, especially during their stay in a confined room due to their medical and physical needs. With a physical therapy bed rails assessment form, a physical or occupational therapist will be able to determine whether or not their patient or an individual will be needing the aid of a rail for his condition. The form contains five sections wherein the last section is for the instructions and workflow to be fulfilled by the therapist.
Physical Therapy Bed Rails Assessment Form
The first section is the client information section wherein the personal data of the client or the patient will be indicated including the date when the form and the bed rails are requested for aid and the diagnosis for the patient or his medical condition. The second section consists of questions or simply a medical questionnaire which must be answered by the therapist. The questions center on the functionality of the bed rails for the patient, a list of possible alternatives to be tried by the patient, and whether the patient owns a piece of similar equipment or not. The recommendation and the signature of the therapist will be in the third and fourth sections of the form.
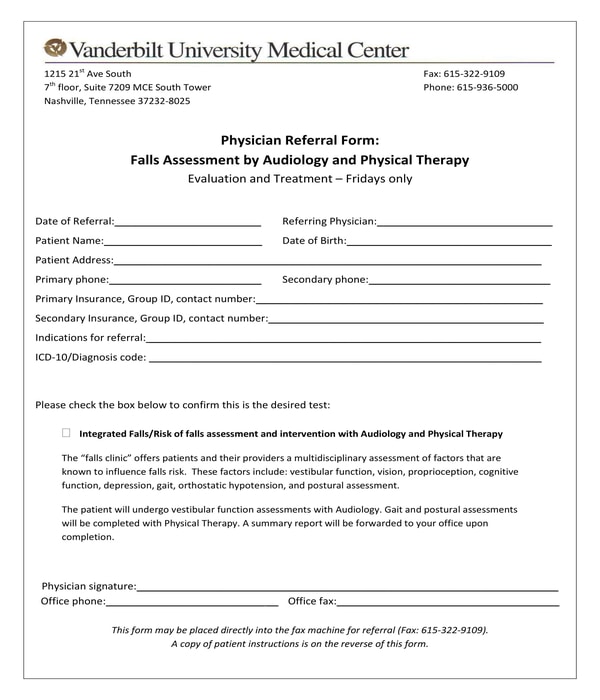
Physical Therapy Falls Assessment Physician Referral Form – If an individual is dealing with a medical condition which increases the risks of him falling, he should be referred by a physician to undergo a physical therapy falls assessment session with a licensed professional therapist. In order to refer a patient, a physical therapy falls assessment physician referral form must be filled out and be signed by the individual’s or the patient’s physician who conducted an initial observation to his case.
Physical Therapy Falls Assessment Physician Referral Form
There are three main sections in a physical therapy falls assessment physician referral form along with an enclosed patient instructions sheet. The date when the referral was conducted, the name of the referring physician, the name and address of the patient, as well as the patient’s date of birth, address, contact information, and insurance details are the information to be stated in the first section of the form. Then, the physician must mark a check on the intended box for indicating that the patient indeed needs to undergo the assessment specified in the form. And with the physician’s signature, office number, and the date when the physician used the referral form must be included to simply complete the referral.
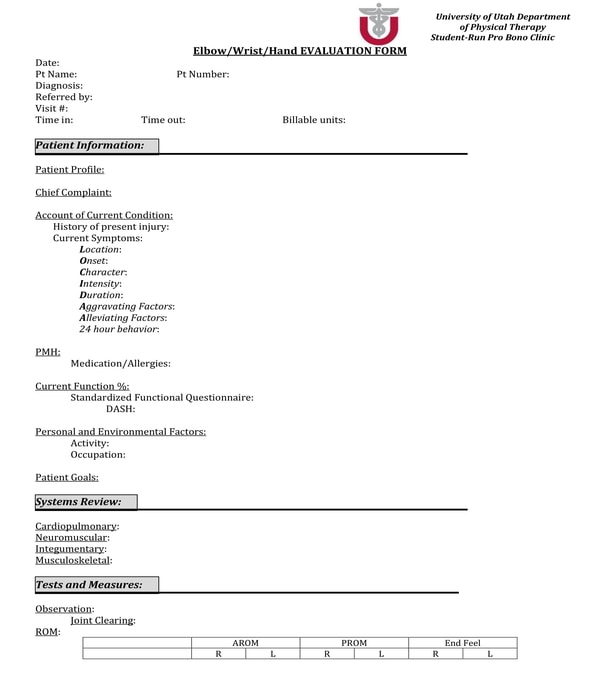
Physical Therapy Hand Evaluation Assessment Form – There are physical therapists whose main body part focus is the hands of their patients which includes the patient’s wrists and elbows. For these therapists, the variety of document to use for documenting their assessments is known as the physical therapy hand evaluation assessment form. There are seven sections in this type of document which are also important to be filled out by the patient and his therapist to collect information to be used for his healing and cure in relation to his physical condition.
Physical Therapy Hand Evaluation Assessment Form
The first section or part of the form is for indicating the date when the assessment was taken by the patient, the patient’s number and name, the diagnosis of the patient and the name of the referring person, the billable units of the patient, and the patient’s time in an out in the medical center or clinic. Then, a patient information section will be the next portion to be completed which is basically for the patient’s profile, complaints, medication and allergies, activities and occupation, and the goals of the patient during his therapy. After which, the systems review of the therapist for the patient will be the focus of the third section of the form while the fourth section enlists the tests and measures of the patient, the fifth section is allotted for the therapist’s evaluation, the sixth section explains the intended plans for caring for the patient, and the seventh section of the form is where an informed consent statement is incorporated for documenting that the patient and his legal guardian were informed of all the treatments and tests conducted by the therapist for the purpose of the assessment.
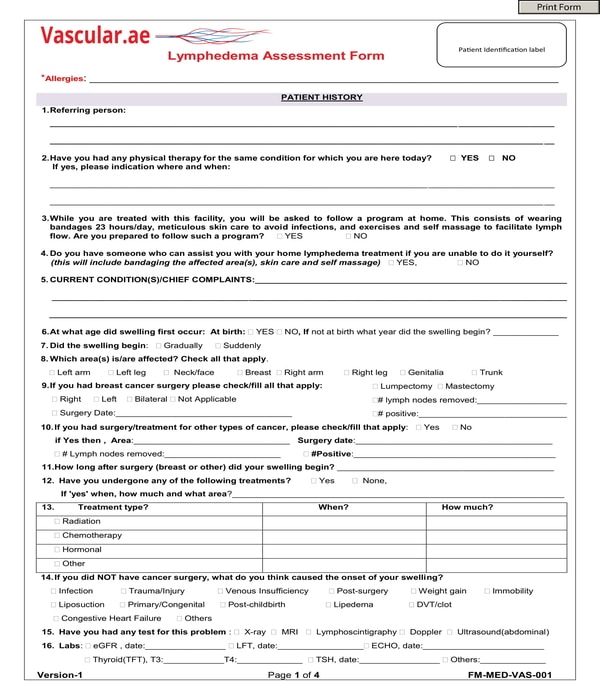
Physical Therapy Lymphedema Assessment Form – Lymphedema patients deal with swollen parts in their bodies, specifically in the arms and legs. To document or record the assessments of a therapist for a lymphedema patient, a physical therapy lymphedema assessment form will have to be used by the therapist. This document mainly consists of questions related to the patient’s needs, condition, treatments and relevant histories to be considered as the possible cause of the patient’s physical state.
Physical Therapy Lymphedema Assessment Form
There is also a section in a physical therapy lymphedema assessment form which contains a set of table and diagrams. The table is for the reviews of the patient’s system, and the diagrams are for labeling purposes for the patient’s pain assessment and swelling location.
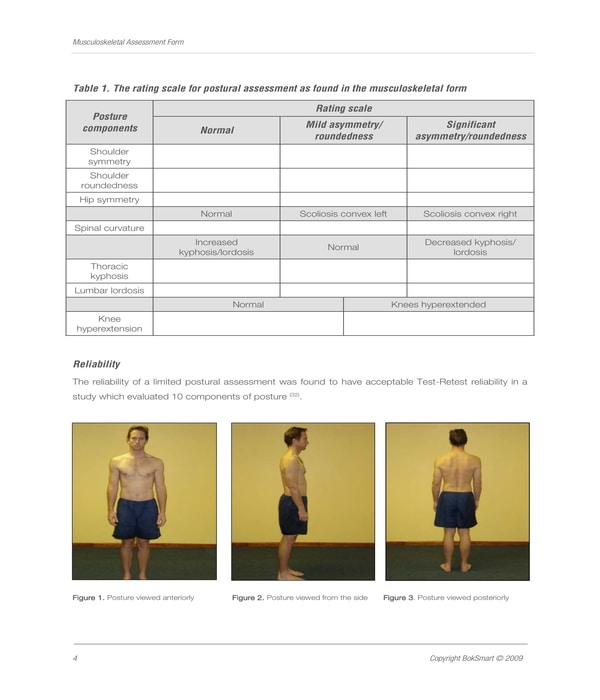
Physical Therapy Musculoskeletal Assessment Form – Musculoskeletal screenings are often mandated to be undergone by athletes and extreme sports enthusiasts, as well as sports coaches and referees. The purpose of a musculoskeletal screening is to ensure the safety of a participant before he gets involved in any type of sports and activities which can put his life at risk. A physical therapy musculoskeletal assessment form is the document to be used by a therapist or a physician who is observing and assessing the athlete. Basically, in the form, the patient’s posture and reliability will be the areas to be assessed by the therapist by using a rating scale or scoring method.
Physical Therapy Musculoskeletal Assessment Form
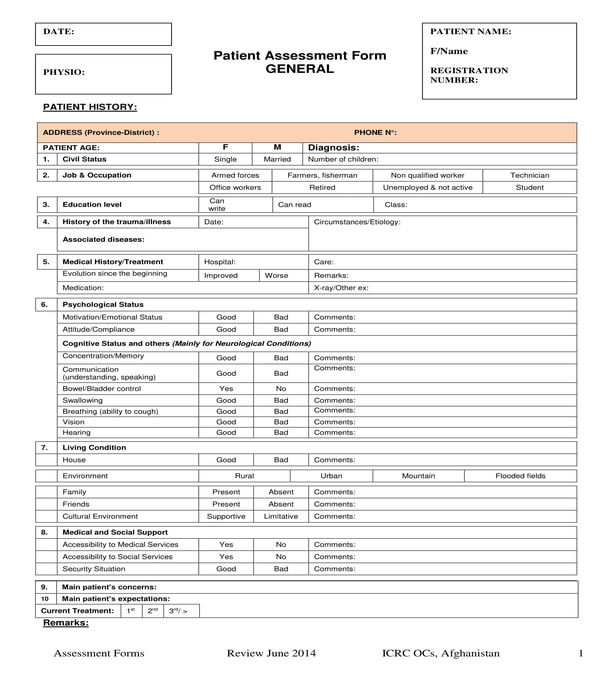
Physical Therapy Patient Assessment Form – This is the most common variety of physical therapy assessment form that therapists use for their patients since it collects general details which are useful for the procedure of determining the cause, treatments, and needs of the patient. Seven sections comprise this type of form. The first section is primarily for the patient’s history which includes the patient’s medical history, psychological status, living condition, and the patient’s medical and social support. In the second section, the patient’s physical examination results will be disclosed using a diagram and sets of tables for the tissue problems of the patient, and the patient’s senses and reflexes.
Physical Therapy Patient Assessment Form
Neurodynamics information, the range of motions that the patient can perform, the patient’s muscle test results, and the details of the patient’s muscle tones will be the focus of the third section of the form. The therapist’s functional evaluation of the patient including gait analysis and the activity restrictions list for the patient are stated in the fourth section while the fifth section will have the conclusions and the findings for the patient’s condition. Moreover, the detailed treatment plan of the therapist and a therapy followup section will be the contents of the sixth and seventh sections of the physical therapy patient assessment form.
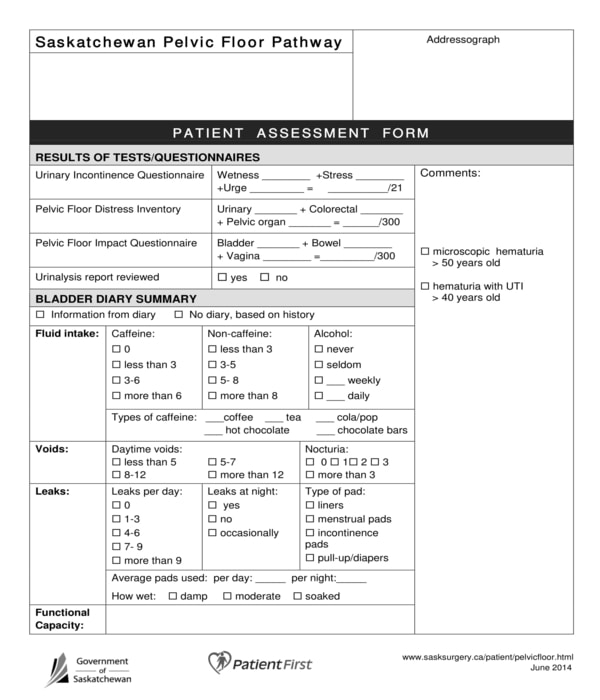
Physical Therapy Patient Pelvic Floor Assessment Form – In this type of physical therapy assessment form, the therapist and the patient will have to complete eight sections for addressing the patient’s physical concerns. The results of the tests and medical examinations that the patient took will be indicated by the therapist in the first section of the form wherein comments and notes can be placed beside it. Then, a bladder diary summary of the patient will be the center of the second section of the form which will be for documenting the liquid intake of the patient and his voids, leaks, and bladder functional capacity.
Physical Therapy Patient Pelvic Floor Assessment Form
A question regarding the patient’s main complaint of his pelvic floor and his bladder will be the content of the third section of the form while the patient’s bladder concerns and red flags will be discussed in the fourth section. The bowel information of the patient will be the focus of the fifth section and other details are to be described in the sixth section, while the seventh and eight sections are for the physical exam record of the patient, and the identified problems of the patient. In addition, there is also a large area in the form which will be for the notes of the therapist and also for his signature and date when he assessed the patient.
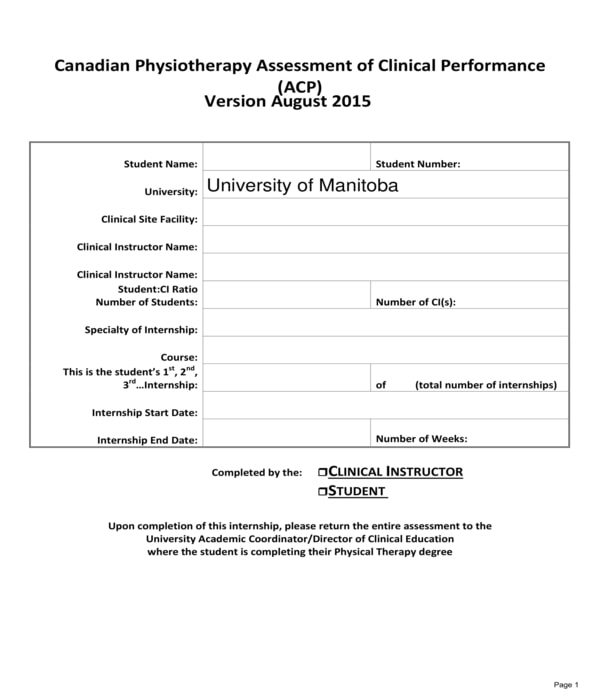
Student Physical Therapy Assessment Form – Students who are taking up courses in physical therapy will be the users of a student physical therapy assessment form. Essentially, the form is to be used only after the internship or the on-the-job training of a student is accomplished. In the form, the name of the student and his identification number will be stated along with the location of the clinical site or facility where he took his internship, the name of his internship instructor, the specialty of the internship, as well as the number of student interns that the instructor is managing throughout the internship period. The date when the internship started and have ended will also be needed to be stated in the form.
Student Physical Therapy Assessment Form
What is Included in the PT Assessment?
- Patient History Review: Examining the Patient Assessment Form to understand past medical history, current symptoms, and goals.
- Physical Examination: Assessing mobility, strength, balance, and pain levels.
- Functional Assessment: Utilizing the Functional Behavior Assessment Form to evaluate daily living activities.
- Special Tests: Conducting specific tests to diagnose or rule out conditions.
- Goal Setting: Collaborating with the patient to set achievable rehabilitation goals.
How to Write a Physical Therapy Assessment?
- Begin with Patient Information: Start by documenting basic information from the Health Assessment Form.
- Summarize the Patient’s History: Highlight key points from their medical and therapy history.
- Detail the Physical Examination Findings: Include results from mobility, strength, and pain evaluations.
- Outline Assessment Results: Use the Functional Behavior Assessment Form findings to summarize functional capabilities.
- Set Treatment Goals: Clearly define short-term and long-term rehabilitation goals.
- Plan of Care: Propose a therapy plan, including types of interventions and frequency.
How do you Conduct a PT Assessment?
- Review Patient History: Gather comprehensive information via the Psychosocial Assessment Form and other relevant documents.
- Perform a Physical Examination: Evaluate physical capabilities and limitations.
- Assess Functional Performance: Utilize the Fitness Assessment Form for an overall fitness evaluation.
- Identify Problem Areas: Focus on specific concerns highlighted in the Nutrition Assessment Form and related assessments.
- Set Goals with the Patient: Use the initial findings to establish rehabilitation objectives.
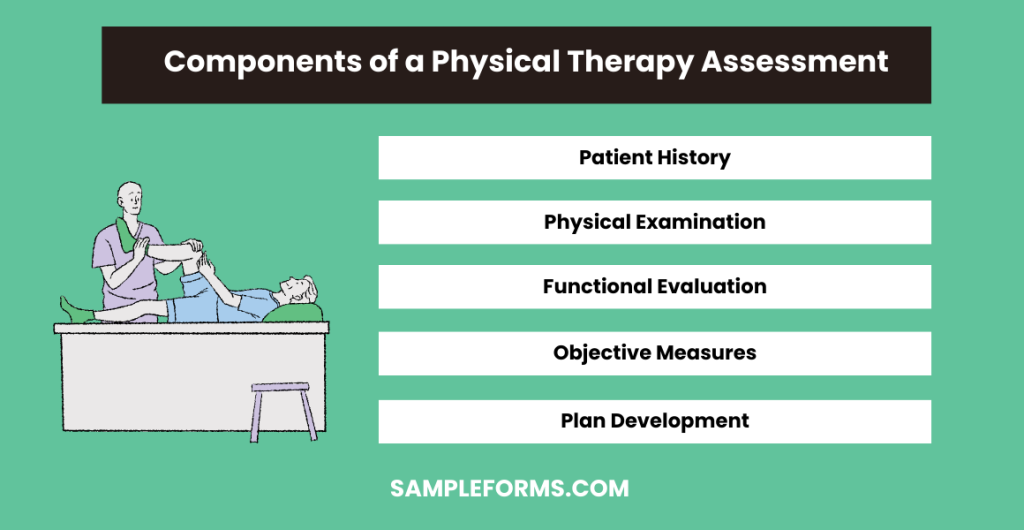
What are the Components of a Physical Therapy Assessment?
- Patient History: Extracted from the Mental Health Assessment Form and similar records for a holistic view.
- Physical Examination: Includes tests for mobility, strength, and pain threshold.
- Functional Evaluation: Using tools like the Skills Assessment Form to gauge daily living skills.
- Objective Measures: Applying standardized tests for specific conditions.
- Plan Development: Formulating a tailored treatment plan based on the assessment.
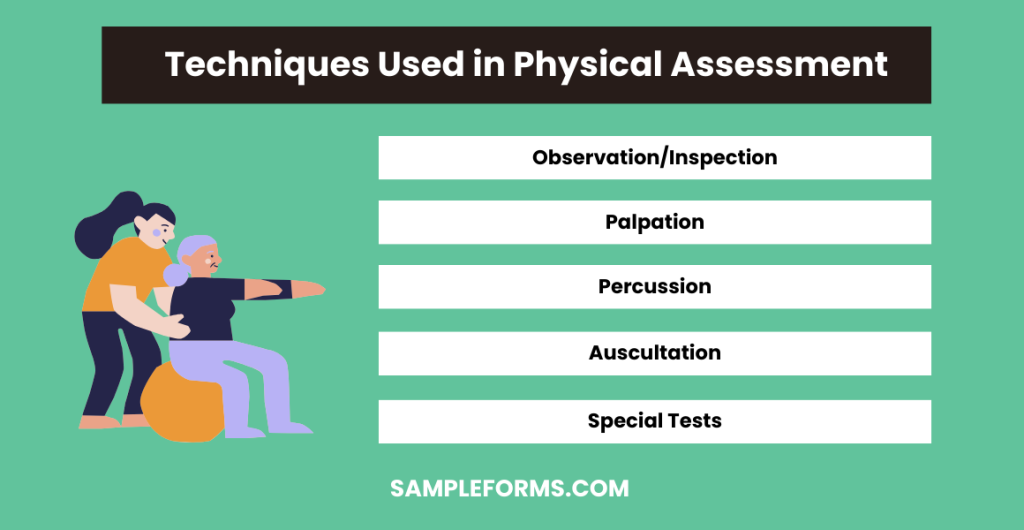
What are the Five Basic Techniques Used in Physical Assessment?
- Observation/Inspection: Utilizing the Teacher Assessment Form approach to observe posture, movement, and behavior.
- Palpation: Feeling the body to identify abnormalities or confirm findings from the Health Assessment Form.
- Percussion: Tapping on the body surface to determine the underlying structure.
- Auscultation: Listening to the body’s sounds for clues about the health of organs.
- Special Tests: Implementing specific diagnostic tests to further investigate findings, similar to strategies used in the Preschool Assessment Form.
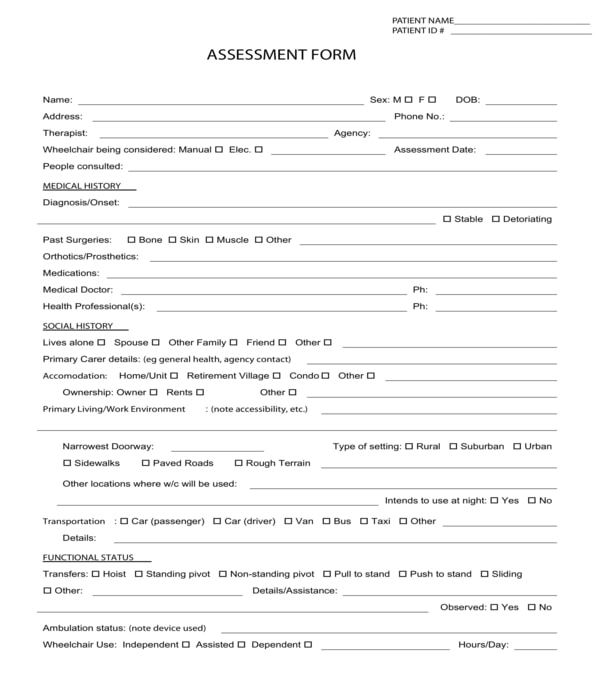
Important Sections in Physical Therapy Assessment Forms
Although there are different types of physical therapies that therapist’ can offer to their patients depending on their professional expertise on the patient’s needs and wants, each physical therapy assessment form to be filled out for the patient must have all the essential or important sections to collect relevant details about the patient’s condition:
- Patient information – Basically, this section of the form is for disclosing the personal data of the patient such as his name, address, contact details, and the patient’s identification number. In addition, the name of the patient’s former therapist and his office address and phone numbers can also be included in this section as well as the other people whom the patient have consulted with regards to his physical condition and needs. You may also see our Community Assessment Form.
- Medical history of patient – Knowing the patient’s medical history is one of the goals of therapists in using a physical therapy assessment form since it allows them to obtain the medical and health background of the patient such as the diagnosis of the patient’s physicians about the patient’s condition, the types of surgeries that the patient had, and whether the patient’s condition is becoming severe, deteriorating, or is stable. You may also see Family Assessment Form.
- The social history of patient – The reason for acknowledging the patient’s social history is to identify possible causes for the patient’s condition which are related to the patient’s behavior and social status. In the social history section of the form, the patient’s living condition of whether he is living alone, living with a spouse, or a family relative and a friend will be identified as well as the name of the patient’s primary care provider if the patient is assisted by a caregiver for his everyday tasks and movements. Moreover, where the patient is residing in including the type of place that he is living, the transportation that he takes every day, and the address of his work or office must also be disclosed in this section of the form. You may also see Capacity Assessment Form.
- Functional status of patient – This section is where the patient can disclose his physical functional status ranging from his ability to stand and sit, up to details of whether he needs a wheelchair and a railing to hold on to for standing or not. If the patient needed the aid of a wheelchair and any medical device, then the number of hours that the patient can sustain without the device is needed to be stated in the form as well to know the patient’s capacities and limitations. You may also see our Driver Assessment Form.
Additionally, the type of meal plan that the patient is following will also be included to be disclosed in the functional status section along with the communication method preference of the patient, bed mobility and dressing needs, and the other activities that the patient is able to do even with his physical condition. You may also see our Fall Risk Assessment Form.
- Physical evaluation of patient – This section is where the patient or his physician can indicate a physical evaluation observation. Determining the types of visual aids that that patient needs and is using, the patient’s chosen method of communicating, whether the patient has impaired hearing or is deaf, and the skin condition of the patient are some of the information to be focused in this section of the form. You may also see our Hazard Assessment Form
- Patient physical dimensions – Physical therapists need to measure their patients in order to further obtain information about the patient’s physique. Some of the parts to be measured includes the patient’s head and whether it is flexed or extended, as well as the patient’s shoulders and knees. It is also important that the physical therapist will describe his measurements and the movements of the patient such as his reflexes and the tone of his muscles. You may also see our Construction Risk Assessment Form.
Aside from the patient’s physical dimensions, this section can also include an area for disclosing the patient’s wheelchair history and information wherein the specifications of the wheelchair that the patient is using will be stated along with the wheelchair and seating dimensions of the patient. You may also see our Child Assessment Form.
- Patient goals and concerns – Not only the thoughts, observations, and the comments of the physical therapist should be written in the physical therapy assessment form but also the patient’s input about his condition. For this, a section for the patient’s goals and concerns should be incorporated into the assessment form. This will be the section where the patient can explain what he is thinking of and make the therapist aware of his other concerns, related or not related to his physical state or physique. You may also see Pre-Training Assessment Form.
- Physical therapist’s plan – A physical therapy assessment form acts similarly to a patient intake form, however, the difference is that the therapist will have to input his plans in the assessment form to inform the patient, be it a short-term or a long-term plan. After laying down the plans and explaining each item to the patient, the therapist must be able to affix his signature in the assessment form, specifically in an allotted signature block. You may also see Fire Risk Assessment Form.
How do you know if a Physical Therapist is Good?
A good physical therapist has strong communication skills, a personalized approach, positive patient testimonials, and uses the Needs Assessment Form to tailor treatments. Also check our Training Assessment Form.
Can a Physical Therapist write a Doctors Note?
Yes, physical therapists can write a doctor’s note for work or school absences, using insights from the Medical Assessment Form to justify medical leave.
Can a Physical Therapist Diagnose an Injury?
Physical therapists can diagnose musculoskeletal injuries, utilizing the Student Assessment Form to evaluate and plan appropriate treatment strategies.
How many Times a Week should you go to Physical Therapy?
The frequency depends on your condition, with a typical range of 2-3 times a week, guided by evaluations from the Training Needs Assessment Form.
When Should you Stop Physical Therapy?
You should stop physical therapy when you’ve met your goals, upon advice from your therapist, or if there’s no improvement, as assessed by the Restaurant Risk Assessment Form.
What is the Average Number of Visits for Physical Therapy?
The average number of visits varies, usually between 6 to 12 sessions, depending on the injury’s severity and progress monitored through the Fire Risk Assessment Form.
In conclusion, the Physical Therapy Assessment Form is an indispensable resource in the realm of physical therapy, facilitating thorough evaluations and informed treatment decisions. Through the use of samples, forms, letters, and practical advice, healthcare providers can ensure a comprehensive intake process. This guide underscores the significance of the Physical Therapy Intake Form, highlighting its role in capturing essential patient information and setting the stage for successful rehabilitation outcomes.
Related Posts
-
Content Retention Through Assessment Form [ How to, Importance, Tips ]
-
Enquiry Form
-
FREE 5+ Recruiter Performance Review Forms in PDF | MS Word
-
Job Safety Observation Form
-
FREE 4+ Hazard Observation Forms in PDF
-
FREE 5+ Coach Observation Forms in PDF | MS Word
-
FREE 4+ Child Care Observation Forms in MS Word | PDF
-
FREE 4+ Child Observation Forms in PDF | MS Word
-
Preschool Observation Form
-
Student Observation Form
-
Peer Observation Form
-
Lesson Observation Form
-
Assessment Form
-
The Importance of Risk Assessment and Safety Statement [ What Is, How to Conduct ]
-
Risk Assessments And Safety Statements Guidelines [ What Is, Process ]